Stay up to date with news about TIME-AD!
Postdoctoral Research Position in Biostatistics
The Department of Epidemiology and Biostatistics at UCSF is seeking a highly motivated postdoctoral researcher to support the TIME-AD Analytics Core. This position offers a unique opportunity to work on cutting-edge statistical methodology, with an emphasis on causal inference and information synthesis, closely linked to applications in cognitive aging research.
AAIC Abstract Submissions
AAIC will be held in London, United Kingdom and online from July 12-15, 2026. The deadline for abstract submissions is January 12th.
Submit an abstract or session proposal for the opportunity to feature your work among 4,000 posters and 800 podium presentations on the latest dementia research. AAIC welcomes submissions on basic science and pathogenesis, biomarkers, clinical manifestations, drug development, public health, dementia care and more.
Click this link for submission information!
SER Abstract Submissions
The Society of Epidemiologic Research (SER) 2026 Annual Meeting will take place in Phoenix, Arizona from June 23-26, 2026. The deadline for abstract submissions is January 13th.
SER’s Annual Meeting brings together epidemiologists from around the world for a dynamic four-day experience of learning, connection, and celebration. Participate for an opportunity to share research, attend workshops, and connect with experts from around the world.
Click this link for more information!
UCSF Dementia Day
Sandler Neurosciences Center
Dec 8 from 9:30am to 4:30pm PST
The fifth annual UCSF Dementia Day will be held in person from 9:30am – 4:30pm on Monday, December 8, 2025, at the Sandler Neurosciences Center. It will include expert speakers and a poster session, and the featured themes will include diagnosis, care management, caregiver support, and transitions of care and end of life. This event is free and open to the UCSF community. Abstracts are due by December 1, 11:59 PM.
To submit your abstract, please click here.
To register for the event, please click here.
TIME-AD All Personnel Meeting
On November 7, 2025, TIME-AD held a successful all-personnel meeting to align and prepare for GSA 2025. The meeting featured key program updates, an open Q&A, and practice presentations from team members who presented at the conference
TIME-AD at GSA:
Maria Glymour and Sarah Ackley presented at “The Biggest Baddest Bias in Aging Research”
Paloma Rojas-Saunero presented “Causal Estimands for Aging-Relevant Outcomes in the Presence of Death as a Competing or Truncating Event”
Ruijia Chen presented "Social Isolation and Cognitive Aging: Are Operational Definitions Creating a Reproducibility Crisis?"
Yulin Yang presented “Social isolation prevalence estimates and trends over time: it depends on what you measure”
Ashwin Kotwal presented “Unseen and Undiagnosed: The Relationship of Social Isolation to Underdiagnosed Dementia” during the symposium “Social Networks in Dementia”
Gina Nam presented the poster “Classification Matters: Divergent Estimates of Dementia Risk Factors in the Health and Retirement Study”
New TIME-AD Publication:
Estimating preclinical amyloid positivity: A case study transporting ADNI to ARIC
Published in Alzheimers & Dementia
Alzheimer's disease and related dementias researchers have benefited from deeply phenotyped clinical samples; however, there is a critical need for estimates that generalize to diverse, representative populations. Use of a statistical approach from causal inference, “transport,” may allow generalization of findings from clinical samples to other target populations. Here we explore the feasibility and validity of extending results from a clinical sample, the Alzheimer's Disease Neuroimaging Initiative (ADNI), to a community-based target sample, the Atherosclerosis Risk in Communities Study Positron Emission Tomography Amyloid Imaging Study (ARIC-PET) using transport estimation and a standard approach, direct standardization, which itself can be considered a simple transport.
Eligible ARIC-PET (n = 343) and ADNI (n = 821) participants were White or Black, with normal cognition or mild cognitive impairment (MCI; 26.5% ARIC-PET, 56.4% ADNI). Estimates of amyloid positivity prevalence were derived from transporting from ADNI to ARIC-PET or standardizing ADNI to ARIC–ET using only sociodemographic characteristics and apolipoprotein E (APOE) ε4 status. Resulting estimates were compared to observed prevalences in ARIC-PET, overall and by age, sex, race, education, APOE ε4 status, and cognitive status.
Approximately half of transported prevalences were closer to observed ARIC-PET prevalences than the crude ADNI prevalences, including in all five subgroups in which crude prevalences differed substantially across cohorts. However, for many subgroups, transported prevalences were substantially further from observed ARIC-PET prevalences than crude ADNI prevalences. Standardization produced more variable estimates, which were not systematically closer to observed ARIC-PET prevalence than the crude ADNI prevalence estimates. Restriction to more homogenous samples did not improve performance of either method.
Although transport performed better than direct standardization in this example, available data appear insufficient to generalize findings from convenience samples to less selected samples with high confidence using either method. Recruitment of diverse, representative samples will likely be needed to derive population-level statistics given limitations of legacy samples.
Spring 2026 TIME-AD Fellowship for Masters Students at Boston University
TIME-AD invites applications from master’s-level Boston University students for a part-time fellowship this spring semester.
Join faculty-led research exploring innovative approaches to understanding and preventing Alzheimer’s disease and related dementias! As a TIME-AD Fellow, you’ll work closely with a dedicated mentor, contribute to meaningful research projects, and present your work at the end of the program. Fellows receive a $1,000 stipend for up to 50 hours of research across the semester or academic year.
Info Session: Thursday, December 4th, 1:00–2:00 PM | Room L-203
Application Deadline: January 11th, 2026 at 11:59 PM
Fellowship Decisions Released: January 16th
Program Begins: January 20th
Have questions? Contact shelliv@bu.edu
New TIME-AD Publication:
Harnessing Geospatial Artificial Intelligence (GeoAI) for Environmental Epidemiology: A Narrative Review
Published in Current Environmental Health Reports
Purpose of review: Geospatial analysis is an essential tool for research on the role of environmental exposures and health, and critical for understanding impacts of environmental risk factors on diseases with long latency (e.g. cardiovascular disease, dementia, cancers) as well as upstream behaviors including sleep, physical activity, and cognition. There is emerging interest in leveraging machine learning and artificial intelligence (AI) for environmental epidemiology research. In this review, we provide an accessible overview of recent advances.
Recent findings: There have been two major recent shifts in geospatial data types and analytic methods. First, novel methods for statistical prediction, combining geospatial analysis with machine learning and artificial intelligence (GeoAI), allow for scalable geospatial exposure assessment within large population health databases (e.g. cohorts, administrative claims). Second, the widespread adoption of smartphones and wearables with global positioning systems and other sensors has allowed for passive data collection from people, and when combined with geographic information systems, enables exposure assessment at finer spatial scales and temporal resolution than ever before. Illustrative examples include refining models for predicting outdoor air pollution exposure, characterizing populations susceptible to water pollution, and use of deep learning to classify Street View image-derived measures of greenspace. While these tools and approaches may facilitate more rapid, higher quality objective exposure measures, they pose challenges with respect to participant privacy, representativeness of collected data, and curation of high quality validation sets for training of GeoAI algorithms. GeoAI approaches are beginning to be used for environmental exposure assessment and behavioral outcome ascertainment with higher spatial and temporal precision than before. Epidemiologists should continue to apply critical assessment of measurement accuracy and design validity when incorporating these new tools into their work.
New TIME-AD Publication:
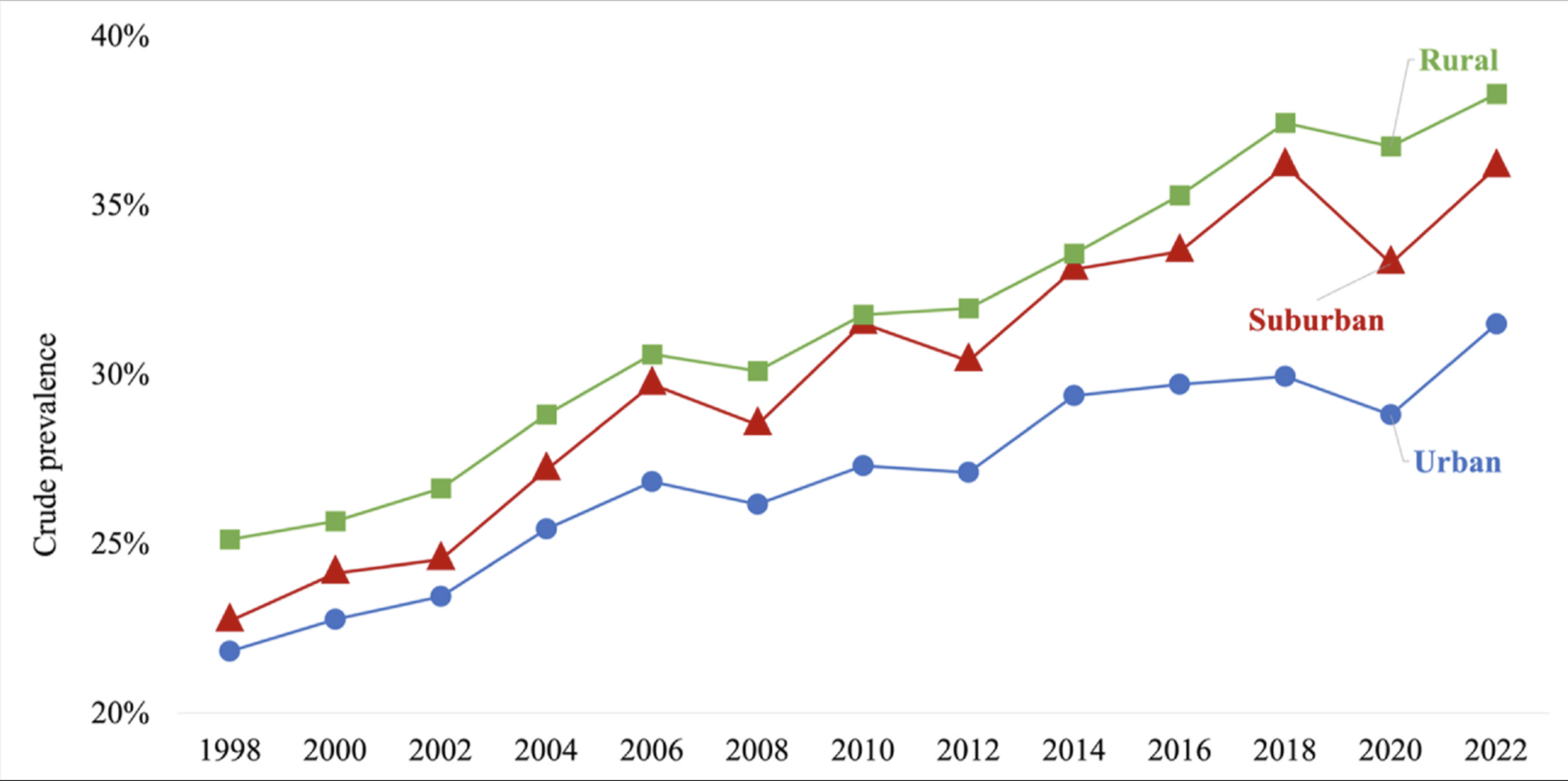
Chronic pain prevalence and trends in urban, suburban, and rural areas among American adults aged 55+, 1998-2022
Published in Social Science & Medicine
Rural-urban health disparities in the United States are large and persistent, yet most surveillance efforts focus on mortality and disability. Monitoring rural-urban trends in pain, a major but overlooked indicator of population health, remains understudied. Given changes in demographics and resources of urban, suburban, and rural areas since the turn of the 21st century, which may have altered place-based differences in pain prevalence. Using nationally representative data from the Health and Retirement Study of 35,230 adults aged 55 and older (n = 206,600 person-wave observations), we estimated pain prevalence and trends across urban, suburban, and rural areas from 1998 to 2022. We assessed variation by age, sex/gender, race and ethnicity, and census region. Over 24 years, pain prevalence increased by 70 % (Prevalence Ratio [PR] = 1.70, 95 % Confidence Interval [CI]: 1.64, 1.75) and was consistently highest in rural areas and lowest in urban areas. However, pain prevalence rose most sharply in suburbs as compared to both rural and urban areas (suburban and time interaction vs. rural areas: PR = 1.08, 95 % CI: 1.00, 1.17). Suburban pain prevalence was similar to urban levels in 1998 but converged with that of rural levels by 2022. Stratified analyses revealed broadly similar patterns across demographic and regional groups, with particularly rapid increases among suburban populations in the South. These findings highlight nationwide increases in chronic pain, with suburban areas emerging as new "hotspots" alongside rural areas. Given that pain is a leading cause of disability and functional decline, monitoring place-based trends is essential for addressing this growing public health concern.
New TIME-AD Publication:
NACC data: Who is represented over time and across centers, and implications for generalizability
Published in Alzheimers & Dementia
Since 2005, the Alzheimer's Disease Research Centers (ADRCs) have recruited participants into the Uniform Data Set (UDS), but enrollment trends and center-level differences remain underexplored. This study investigates temporal patterns and heterogeneity in recruitment across ADRCs, with implications for generalizability.
Using data from the National Alzheimer's Coordinating Center (NACC), we assessed trends and between-center variation in baseline characteristics, including age, sex, race, education, clinical diagnosis, referral source, family history, and co-participant relationship.
All characteristics except sex and family history showed directional shifts over time. Substantial between-center heterogeneity was observed in all variables examined.
Temporal changes and site-level variability in participant profiles highlight challenges and opportunities for generalizing findings from UDS data. Although not nationally representative, statements about generalization could often be made using UDS data, with strengthened inferences and enhanced transparency through analytic approaches such as sensitivity analysis or meta-analytic techniques treating centers as separate studies.
New TIME-AD Publication:
Cognitive data harmonization across two racially diverse cohorts in the United States
Published in Alzheimer's & Dementia: Behavior & Socioeconomics of Aging
Few cohorts have sufficient diversity to identify drivers of racial disparities in cognitive aging. Pooling data from different samples can increase sample size and diversity.
We statistically harmonized cognitive function data from two US cohorts: 2010 Health and Retirement Study (HRS; n=18,422) and 2009-2013 Reasons for Geographic and Racial Differences in Stroke waves (REGARDS; n=19,690). We used confirmatory factor analysis (CFA) to derive harmonized scores for general and domain-specific cognitive function, leveraging common cognitive test items across studies and retaining those unique to each study. We assessed validity of the cognitive scores by regressing them on age, sex/gender, and education.
The combined sample had a mean age of 67.69 (SD=10.22) years. CFA models had good fit. Harmonized cognitive scores demonstrated good criterion validity.
Pooled analyses of harmonized cognitive scores are a feasible means to increase cohort diversity for understanding drivers of racial disparities in cognitive aging.
New TIME-AD Publication:
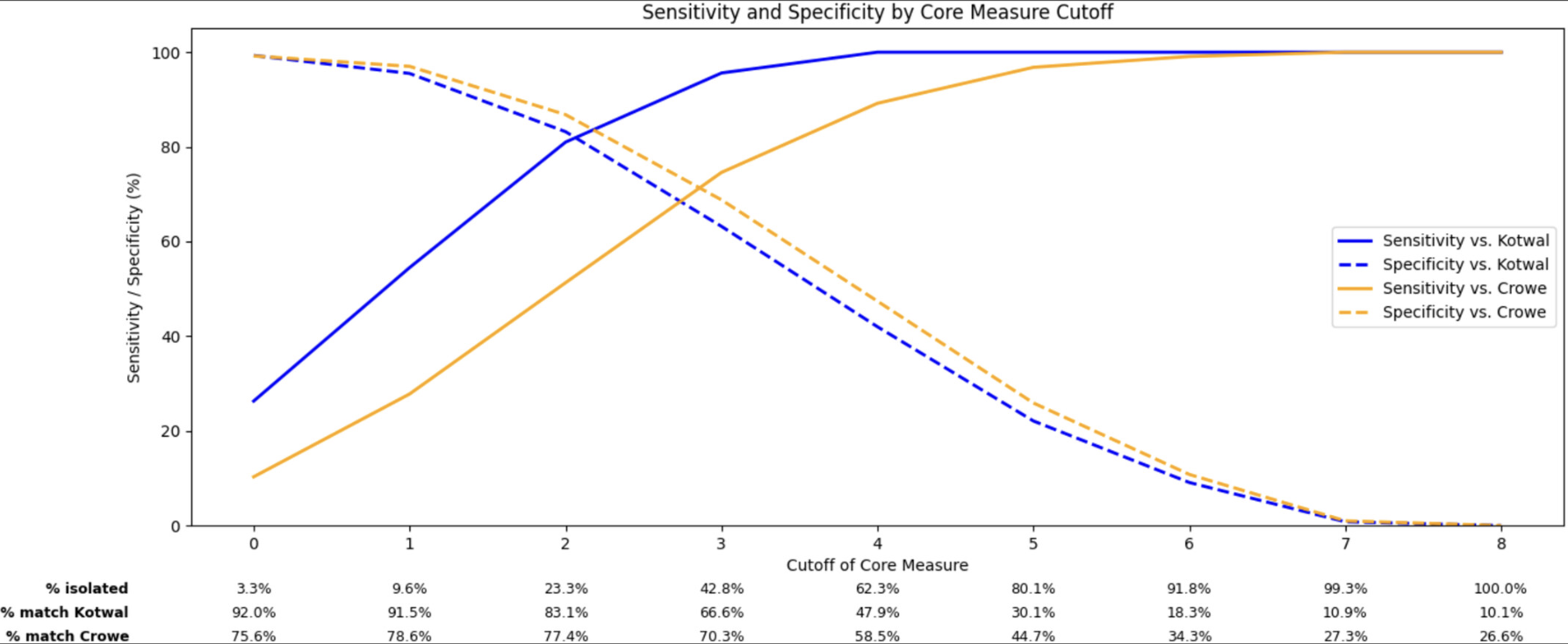
Development and Evaluation of a Brief Social Isolation Measure in the Nationally-Representative Health and Retirement Study
Published in Journal of the American Geriatrics Society
The Health and Retirement Study (HRS) has been central to identifying social isolation as a key determinant of health among older adults. However, prior HRS social isolation measures have relied on a subset of participants responding to a leave-behind questionnaire (LBQ), which limits longitudinal analyses, sample size, and inclusion of individuals with cognitive impairment who require a proxy. This study developed a brief social isolation scale that can be used in the full HRS cohort.
We used 2016 and 2018 HRS data, including 6122 adults ≥ 65 years old. The brief 5-Item "Core" Social Isolation Measure (Range: 0-8 Points) Included Items From the HRS core interview administered to all respondents: marital status, household size, proximity to children, religious participation, and volunteering. We compared three cutoffs (≤ 1, ≤ 2, ≤ 3) to cutoffs for previously established scales (Kotwal and Crowe) Using Sensitivity, specificity, and overall classification accuracy. We also compared the prevalence across demographic and health subgroups, and construct validity through associations with loneliness, depressive, symptoms, and life satisfaction.
Participants were on average 75.4 years old (SD 7.2), 60% women, and 10% socially isolated using the Kotwal measure and 27% using the Crowe measure. A core measure cutoff of ≤ 2 correctly classified 83.1% vs. Kotwal (Sensitivity: 81.0%, Specificity: 83.2%) and 77.4% vs. Crowe (51.3%, 86.8%). At cutoff ≤ 3, accuracy was 66.6% vs. Kotwal (95.6%, 63.2%) and 70.3% vs. Crowe (74.6%, 68.8%). All three measures showed strong construct validity with loneliness, depressive symptoms, and life satisfaction, and relatively consistent prevalence estimates across sociodemographic and health groups.
A Brief Social Isolation Measure Aligns Well With Longer, Previously-Established Measures While Addressing Key Limitations in Data Availability and Sample Representativeness. Researchers Should Consider the Appropriate Cutoff Depending on the Research Context, and the Relative Importance of Sensitivity, Specificity, and Sample Size.
New TIME-AD Publication:
Independent and joint associations of key social exposome components with cognitive aging: triangulating evidence through cross-national data
Published in the American Journal of Epidemiology
We examined the independent and joint associations of five key social exposome components, including financial strain, neighborhood disorder, perceived discrimination, social strain, and traumatic life events, with cognitive function levels and decline. Data were from adults aged > 50 in the US Health and Retirement Study (HRS; n = 13 795; 2008-2020) and the English Longitudinal Study of Aging (ELSA; n = 9469; 2006-2019), and adults aged ≥65 in their Harmonized Cognitive Assessment Protocol (HCAP) subsamples (HRS-HCAP: n = 2749; 2016; ELSA-HCAP: n = 955; 2018). Using linear mixed-effects models and quantile-based g-computation, we found that all components, except traumatic life events, were associated with lower cognitive function. Simultaneously lowering all components by one quartile could improve cognitive function by 0.10 SD units (95% CI, 0.08-0.12) in the HRS, 0.13 SD units (95% CI, 0.10-0.16) in the ELSA, and 0.08 SD units (95% CI, 0.03-0.14) in the HRS-HCAP. Neighborhood disorder had the strongest negative association with cognitive function in the United States, while financial strain had the strongest association in England. No social exposome components were associated with faster cognitive decline. The associations of key social exposome components with cognitive function were consistent across countries, although the magnitude of the joint association was greater in England.
New TIME-AD Publication:
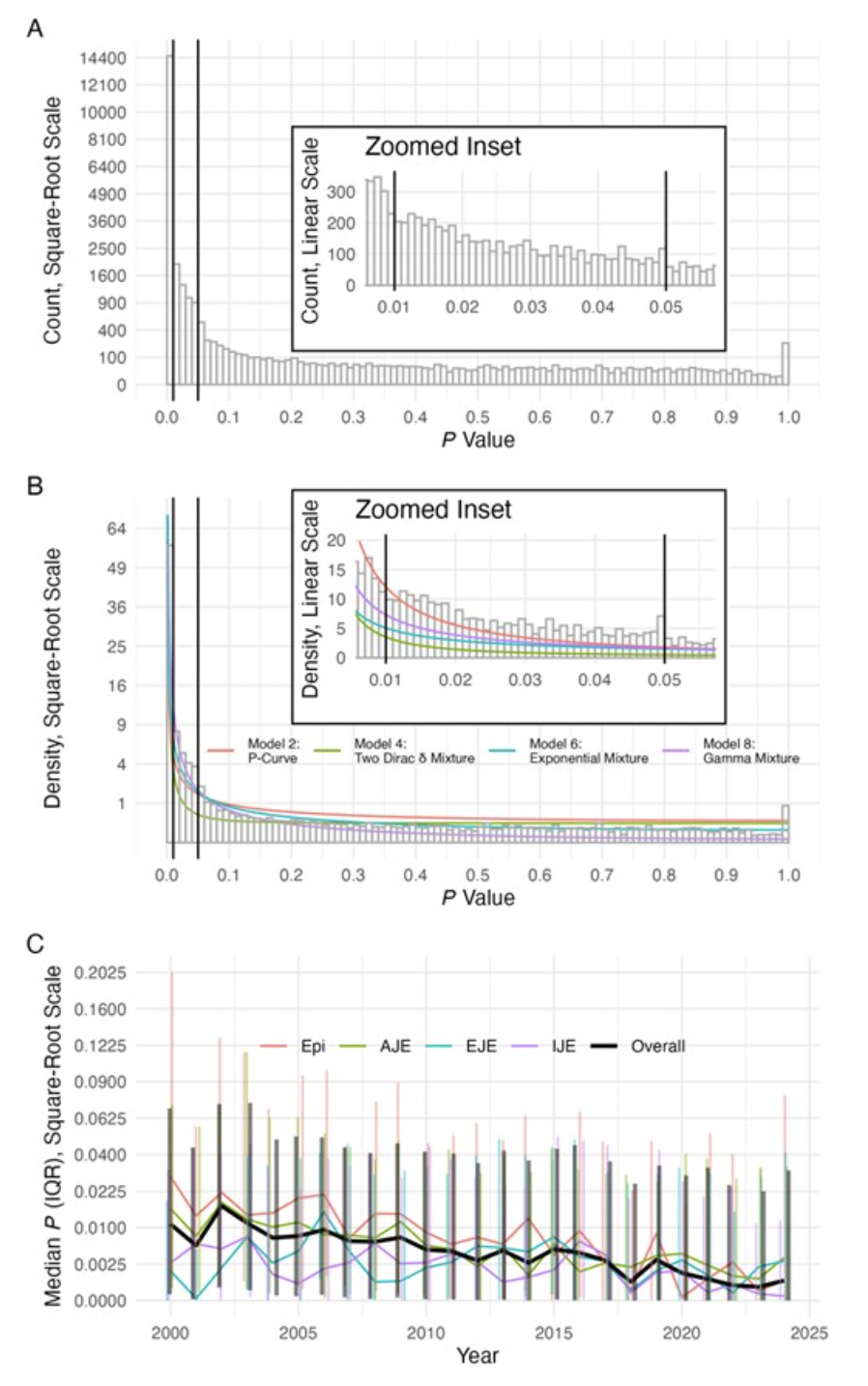
Trends in the distribution of P values in epidemiology journals: a statistical, P-curve, and simulation study
Published in the American Journal of Epidemiology
Epidemiologists have advocated for reporting confidence intervals and deemphasizing P values to address long-standing concerns about null-hypothesis statistical-significance testing, P hacking, and reproducibility. It is unknown if efforts to reduce reliance on P values have altered the distribution of P values. For 21 332 abstracts published 2000 to 2024 in 4 major epidemiology journals, two-sided P values (N = 25 288) were calculated from estimates and confidence intervals scraped using ChatGPT's 4o-mini model. We evaluated trends over time to determine whether the empirical distribution of P values changed. We fitted to expected P-value distributions and simulated these distributions with and without assuming changes in statistical power over time. Average P values decreased from 2000 to 2024; the fraction of P values just below the .05 threshold also decreased. Fits to models indicate that statistical power increased. Increasing power would reduce average P value while also decreasing P values near the .05 threshold-precisely the trends observed in epidemiology journals. Although the frequency of P values near the .05 threshold has declined modestly, this likely reflects increases in statistical power rather than decreases in P hacking.
New TIME-AD Publication:
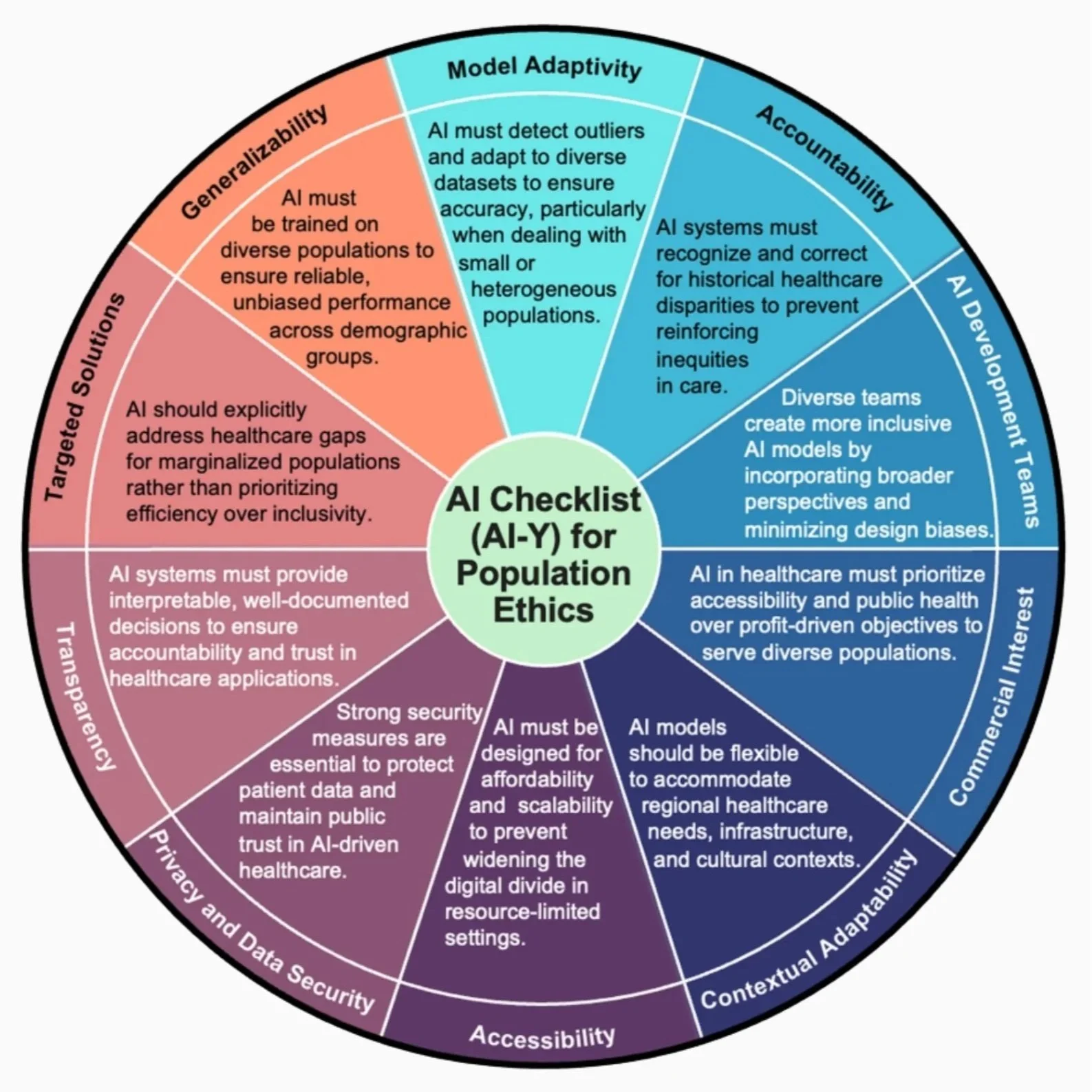
AI-Y: An AI Checklist for Population Ethics Across the Global Context
Published in Current Epidemiology Reports
The goal of this narrative review is to introduce and apply Hswen’s AI Checklist (AI-Y) for Population Ethics, a structured ethical framework created to evaluate the development and deployment of artificial intelligence (AI) technologies in public health. The review addresses key questions: How can AI be ethically assessed across global healthcare contexts and what principles are needed to ensure contextually appropriate AI use in population health.
Recent research highlights a significant disconnect between AI development and ethical implementation, especially in low-resource settings. Studies reveal issues such as homogeneity in the training data, and limited accessibility. Through six global case studies—spanning dementia care in Sweden, environmental forecasting in Europe, suicide prevention in Native American communities, schizophrenia care in India and the U.S., and cervical cancer and tuberculosis diagnosis in Low- and Middle-Income Countries—researchers demonstrate AI’s promise in enhancing preparedness diagnosis, screening, and care delivery while also underscoring ethical gaps in accountability, and governance.
Our examination using the AI-Y Checklist found that ethical blind spots are widespread in the development and deployment of AI tools for population health—particularly in areas of model generalizability, accountability, and transparency of AI decision-making. Although AI demonstrates strong potential to enhance disease detection, resource allocation, and preventive care across diverse global settings, most systems evaluated in our six case studies did not meet key ethical criteria such as access, and localized validation and development. The major takeaway is that technical excellence alone is insufficient; ethical alignment is critical to the responsible implementation of AI in public health. The AI-Y Checklist provides a scalable framework to identify risks, guide ethical decision-making, and foster global accountability. For future research, this framework enables standardized evaluation of AI systems, encourages community co-design practices, and supports the creation of policy and governance structures that ensure AI technologies advance health ethics.
New TIME-AD Publication:
Are we there yet? Estimating the waves of follow-up required for stable effect estimates in cognitive aging research
Published in the American Journal of Epidemiology.
Cognitive aging research relies on longitudinal data, but extended follow-up is costly. The extent to which estimates and precision from data with shorter follow-up diverge from estimates based on longer follow-up is unknown. We evaluated how the length of the follow-up period affects the stability and variance of effect estimates. We also compared estimates derived from models that use current age as the timescale to models that use time-since-baseline, controlling for baseline age. This comparison addresses a significant methodological debate in cognitive aging research regarding how different timescale specifications affect the stability and interpretation of effect estimates. We used data on adults age 65+ from the 2006-2018 U.S. Health and Retirement Study. We estimated linear mixed models for the association of 8 commonly studied dementia risk factors with cognitive decline. We estimated the associations by including an interaction term between the risk factor and time-since-baseline, additionally controlling for baseline age. In separate models, we included an interaction term between the risk factor and current age. We repeated these models across datasets with varying hypothetical follow-up length (1-7 waves, representing 0-12 years of follow-up). We compared coefficients and variance estimates to results from benchmark models (i.e., using 7 waves and/or specifying time-since-baseline). Specifically, we estimate the bias and design effect (i.e., relative variance) of coefficients from models with follow-up periods of 0-10 years (1-6 waves) and/or specifying current age compared to those using 12 years (7 waves) of data in the HRS and/or specifying time-since-baseline.
We found that estimates from models using short follow-up, i.e. 2-3 waves, differed from those derived from models using 7 waves. By 4-5 waves, the bias of coefficients was generally inconsequential. Increased variance with short follow-up was more problematic: using only 2 waves of data, the variance of coefficients was as great as 19 times the variance of corresponding coefficients using 7 waves of data. The greatest improvement in variance was achieved when adding a second or third wave of data, but even with 4 waves of data the variance of coefficients was often several times larger than the variance achieved with 7 waves of data. In models assuming equal follow-up duration, estimates of cognitive change specified by current age differed from estimates using time-since-baseline but were more precise, especially with shorter follow-up. These results offer empirical evidence on the extent to which shorter follow-up may lead to unstable or biased conclusions. Prior guidelines specify that time-since-baseline is preferred over current age for the timescale specification. However, our results demonstrate that using current age substantially increases precision, especially when follow-up periods are short.
New TIME-AD Publication:
The Association of Alzheimer’s Disease Genetic Risk with Social Connectedness in Middle- And Older-Ages
Published in the American Journal of Epidemiology.
Alzheimer’s disease develops during a decades long pre-clinical period prior to diagnosis. Subtle changes in thinking, memory and behavior have previously been shown to emerge during this time. It would require a long-term study in order to observe the associations between in a participant’s 40s or 50s with Alzheimer’s disease diagnoses, which typically occurs after age 65. However, genetics partially predict Alzheimer’s disease. We can better understand the early progression of Alzheimer’s disease by comparing people with a high vs low “genetic risk”.
Using data from the UK Biobank, which includes genetics and survey data for nearly 500,000 UK residents, we found that people who have a higher genetic risk for Alzheimer’s disease were less likely to be socially isolated and reported better family relationships in midlife and early older age than those who had lower genetic risk. We also found no differences in other measures of social engagement, including feelings of loneliness, emotional support, or friendship quality, based on genetic risk for Alzheimer’s disease. These results were not what we expected as withdrawal from social networks has been documented previously. While further research is needed, we hypothesize that those experiencing early symptoms of Alzheimer’s disease are relying more on their support networks due to increased need for assistance with daily activities.
SER Workshop Announcement:
Practical coding to address the reproducibility crisis
Presenters: Scott Zimmerman (Boston University & University of California San Francisco) and Erin Ferguson (University of California San Francisco)
June 10, 2025, 1:00pm – 5:00pm ET
Boston MA
Join us at the Society for Epidemiologic Research annual meeting 2025 in Boston, where we will discuss multiverse analysis, one of the triangulation methods we are using for TIME-AD.
Workshop description:
While replication of results is an essential component of the scientific method, recent work has shown that many findings can not be reproduced. In this context, approaches allowing for rigorous evaluation of how analytic decisions affect estimates are needed. Proposed approaches (e.g. multiverse analyses, multidimensional sensitivity analyses, and simulations sampling from a parameter space) require specifying and iterating over hundreds or thousands of analysis options, models, or datasets. However, little guidance has been provided for how to write and organize code to efficiently iterate over large numbers of specifications.
Using multiverse analysis to investigate how different specifications of eligibility criteria, exposure definition, and covariate sets affect estimates in an applied example in BRFSS, we will provide a framework and example R code for conducting and visualizing analyses where the researcher would like to iterate over many analysis specifications.
Building on R fundamentals, participants will write efficient code to iterate over analytic decisions, yielding organized results. After this workshop, participants will better understand intermediate coding concepts (parallel computing, functions, and loops), efficiently structure code, and successfully complete a multiverse analysis from start (design) to finish (visualization). These skills will improve reproducibility of code and understanding of how analytic decisions impact scientific conclusions.
Evidence Integration Approaches Based on Data Harmonization and Synthetic Data Sets
Evidence Integration Approaches Based on Data Harmonization and Synthetic Data Sets
21st Advanced Psychometric Methods in Cognitive Aging (ΨMCA) Research Conference
August 10 – August 15, 2025
We are accepting applications for the 21st conference on the application of modern psychometric and statistical methods in cognitive aging research. We are planning an in-person conference at Granlibakken Conference Center at Tahoe City, CA for August 10-15, 2025, with a virtual workgroup report and wrap-up session a few months later.
Theme: Integrating findings from multiple data sources is essential for advancing research on cognitive aging and dementia. However, inconsistencies in measurement across studies and restrictions on data access often create major barriers to evidence synthesis. This workshop will explore innovative strategies to overcome these challenges, focusing on two key approaches: data harmonization and synthetic data generation. This workshop will introduce practical tools for combining data from different studies, even when the measurements are not identical. We will cover techniques to make data from different sources more comparable (harmonization) and ways to generate realistic but artificial datasets (synthetic data) to help researchers overcome barriers related to privacy, missing measures, and statistical power. These approaches can improve data sharing and support stronger, more inclusive research on cognitive aging. With increasing computational power, the ability to simulate, synthesize, and harmonize data has become an essential skill for dementia research. This workshop will provide hands-on training in these techniques, using real-world datasets.
The deadline for submitting applications to participate in workgroups is Friday, February 28, 2025. Notification of acceptance will occur by Friday, April 4, 2025.
To submit an application to attend the 2025 meeting, please complete the REDCap application form at: https://mrprcbcw.hosts.jhmi.edu/redcap/surveys/?s=EH98XTX9RP3DJ88N.
Congratulations to TIME-AD MPI Dr. Jacqueline Torres and Co-Investigator Dr. Elizabeth Rose Mayeda on being awarded the Presidential Early Career Award for Scientists and Engineers (PECASE), the highest honor bestowed by the U.S. government on outstanding scientists and engineers early in their careers. Check out this link for more info!
MELODEM 2025 Annual Conference
Applications to participate in this year's MELODEM Annual In-Person Meeting are now open! It will be held in St. James Hotel in Red Wing, MN from Monday, June 23rd to Friday, June 27th, 2025. St. James hotel is a wondrous destination along the iconic Mississippi River. Additionally, its historical atmosphere and proximity to the Minneapolis Saint Paul International Airport makes it a great location for our meeting!
The meeting will follow a 2-part format, as in previous years: (1) a series of presentations with extensive discussion, from Monday, June 23rd to Wednesday, June 25th; and (2) a hands-on data workshop, involving a subset of participants from Wednesday, June 25th to Friday, June 27th. Additional details are embedded within the application form.
To apply to participate, please fill out the form below by Monday, January 27th, 2025, 11:59pm US Pacific Time.
New TIME-AD Publication:
Methods to crosswalk between cognitive test scores using data from the Alzheimer's Disease Neuroimaging Cohort
Published in Alzheimers & Dementia
Studies use multiple different instruments to measure dementia-related outcomes, making head-to-head comparisons of interventions difficult. To address this gap, we developed two methods to crosswalk estimated treatment effects on cognitive outcomes that are flexible, broadly applicable, and do not rely on strong distributional assumptions.
We present two methods to crosswalk effect estimates using one measure to estimates using another measure, illustrated with global cognitive measures from the Alzheimer's Disease Neuroimaging Initiative (ADNI). Specifically, we develop crosswalks for the following measures and associated change scores over time: the clinical dementia rating scale sum of box (CDR-SB), Montreal Cognitive Assessment (MoCA), and Mini-Mental State Examination (MMSE) scores. Finally, a setting in which crosswalking is not appropriate is illustrated with plasma phosphorylated tau (p-tau) concentration and global cognitive measures.
Given the inconsistent collection and reporting of dementia and cognitive outcomes across studies, these crosswalking methods offer a valuable approach to harmonizing and comparing results reported on different scales.
AAIC Abstract Submissions
The deadline for AAIC abstract submissions is January 27th! AAIC offers unparalleled exposure for your research across the field. Submit your abstract or session proposal for the opportunity to feature your work among thousands of abstracts submitted on the latest dementia research. Highlight your work in front of dementia researchers from around the globe and bring key opinion leaders together to impact the future of the field. Click this link for submission information!
TIME-AD Co-Investigator Dr. Cynthia Campbell presenting at NIAA webinar:
How Does Alcohol Impact the Lives of Older Adults – And What Can We Do About It?
Tuesday, December 3, 2024
9:00–10:00 a.m. PT
As the population of older adults 65 and above expands rapidly, so do the rates of alcohol use and misuse among people within this age group. The body changes as we age, and these changes render people more susceptible to some of the harms that stem from alcohol use. While the percentage of people ages 65+ who consume alcohol each month increased by 16% between 2002-2019, due to the size of the aging Baby Boomer cohort, the actual number of drinkers in that age group increased 80% during that time. These data highlight the need for early intervention and a broad discussion on what we can do to prevent further upward trends.
This webinar will feature three presentations:
· Trends in Alcohol Use Among Older Adults: Katherine Keyes, PhD, Columbia University
· What are the Impacts of Alcohol Use in Older Adults: Sara Jo Nixon, PhD, University of Florida
· What Can We Do About It? Cynthia Campbell, PhD, University of California, San Francisco/Kaiser Permanente Northern California Derek Satre, PhD, University of California, San Francisco
NIH Videocast will present the webinar at https://videocast.nih.gov/watch=5523
Kaiser Premanente Division of Research October 8, 2024
“This is an exciting opportunity to use data from a variety of complimentary sources to better understand the associations between these risk factors — which we already know how to address — and dementia risk,” Gilsanz said.
Read more at: Innovative approaches to prevent dementia funded by $28.8 million federal grant - Kaiser Permanente Division of Research
Boston University School of Public Health September 27, 2024